Screening Combinatorial Pharmacological Therapies for Fragile X Syndrome
Philippe Jacques Mourrain, PhD
Co-Principal Investigator
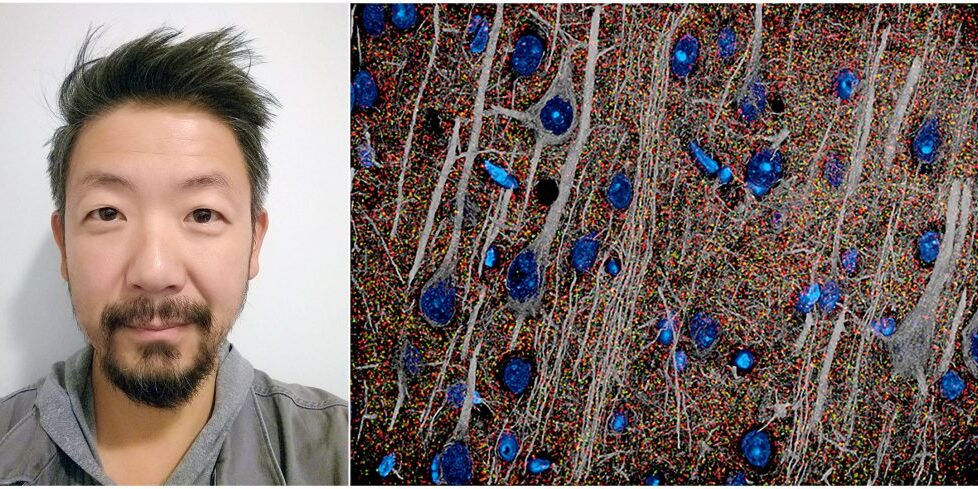
Gordon Wang, PhD
Co-Principal Investigator
Rochelle Coulson, PhD
FRAXA Fellow
Stanford University
Stanford, CA
2021-2023 Grant Funding: $90,000
Summary
There is currently no single treatment that targets all the problems in the brain caused by Fragile X syndrome. This study aims to test different combinations of drugs to see if they can improve the problems in the brain caused by fragile X syndrome in both mouse models and human cells, with the hope of finding a more effective treatment.
The Results
FRAXA-funded researchers at Stanford University explored how ISRIB, an experimental drug, could restore brain function and social behavior in Fragile X syndrome. In Fragile X, neurons struggle to regulate protein production, leading to disrupted learning, memory, and communication between brain cells.
A detailed breakdown of this research is available in our FRAXA research summary. Key findings from the study include:
- Reduced the number of immature dendritic spines, improving brain connectivity.
- Strengthened synaptic function, enhancing neural communication.
- Improved social behavior in Fragile X mouse models.
These findings highlight the potential of targeting underlying protein regulation issues in Fragile X. While ISRIB has not yet been tested in humans for Fragile X, researchers are continuing to study its effects in other conditions, including traumatic brain injury and Alzheimer’s disease. Early-stage human trials are already underway to test ISRIB’s safety and effectiveness in neurological disorders, which could pave the way for future studies in Fragile X.
The team's findings, "Translational modulator ISRIB alleviates synaptic and behavioral phenotypes in Fragile X syndrome", were published in iScience.
The Science
By Philippe Jacques Mourrain, PhD, and Gordon Wang, PhD
Fragile X syndrome (FXS) is caused by the absence of a single protein (FMRP) and is the leading genetic cause of intellectual disability, affecting millions of children worldwide. The loss of FMRP does not produce a singular deficit throughout the brain, but rather a complex array of changes across many brain regions and throughout development.
New therapeutic strategies have immense potential for the improvement of FXS patient quality of life, however there is currently no single therapy that targets the full array of deficits observed throughout the brain. The overall objective of this proposal is to evaluate the additive effects of combinatorial drug treatments to correct a broader spectrum of deficits observed in FXS.
We will achieve this goal through a combination of molecular and imaging techniques, and will take advantage of the unique strengths of both mouse brain and human cell culture models. Through this approach, we will create a map of changes in the brains of both mice and humans caused by loss of FMRP and in response to treatment. This will improve the translational value of the mouse model by providing an accurate measure of how it reflects the abnormalities observed in the human brain.
We will further evaluate the effects of promising drug combinations in human cells from FXS patients, to identify improvements in cellular pathways that underlie the deficits observed in the brain. Importantly, we will assess promising treatments for the development of tolerance, which has proven to be a critical issue in the development of long-term therapeutic approaches.
The use of human FXS cells will improve the clinical significance of our study, allowing us to quickly test a large number of drug combinations in the context of actual patient conditions. Moreover, this analysis opens the possibility that drugs are not tied to a single disease, but to specific deficits, and that a combinatorial approach can be devised to target the array of deficits observed for any neurological disease.
Grant Post Revisions
- 2024/09 - Added The Results
- 2021/05 - Original grant post published.
